Abstract
Background: Platelet transfusions in the United States are increasing in sharp contrast to the marked decrease in red cell and plasma use. Understanding the epidemiology and clinical practice for patients requiring platelet transfusions, particularly in the non-oncologic setting, is needed to identify clinical needs or significant change in practice. Such information can be used to focus the design of evidence based studies to assess platelet transfusion practice and efficacy to areas of high clinical need.
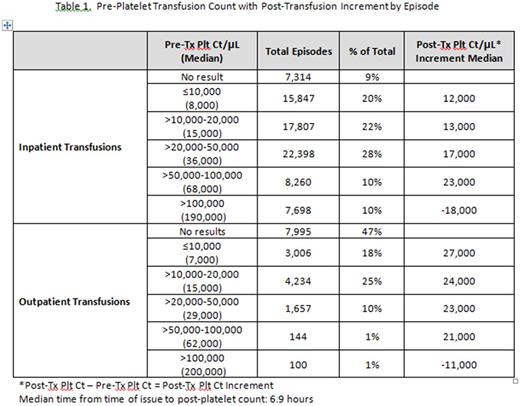
Methods: Patient demographics, laboratory and clinical data were extracted from 2013 - 2015 from blood bank information systems and medical records from 12 REDS-III hospitals (both academic and community) located in four states across the U.S. A patient encounter was defined as any inpatient admission or outpatient visit documented with a unique visit date and discharge date. A transfusion episode was defined as all platelets transfused within an 8 hour interval beginning with the first platelet dose transfused within any encounter. Pre-platelet counts are defined as the nearest count up to 24 hours prior to the first transfusion for inpatients, and up to 48 hours before for outpatients. Post-platelet counts are defined as the first count up to 24 hours after completing the last transfusion for inpatients, and up to 48 hours after for outpatients.
Results: A total of 122,298 platelet doses were issued for transfusion: 74,721 (61%) were apheresis platelets; 47,577 (39%) were pooled whole blood derived platelets; 103,759 (85%) were for inpatients, 18,539 (15%) were for outpatients. For inpatient transfusions 54% were issued to the General Ward, 29% to ICU, 12% to OR, 3% to ER. One platelet dose was issued per episode 78% of the time, 2 doses in 17%, 3 doses in 3%, and 4 doses in 1%. ABO donor-recipient identical platelets were transfused 37% of the time. For selected ABO mis-matched transfusions, type O platelets were given to non-type O patients 8%, and non-type O platelets to type O patients 19% of the time. Cardiovascular, Hematology-Oncology and Gastrointestinal were the most common broad diagnostic categories for encounters. The top three primary ICD 9-10 codes for each of these categories were: Cardiovascular: coronary atherosclerosis of the native coronary artery, aortic valve disorder and intracerebral hemorrhage; Hematology-Oncology: acute myeloid leukemia without achieving remission, neutropenia NOS, and multiple myeloma with achieving remission; Gastrointestinal: alcohol cirrhosis of the liver, cirrhosis of the liver NOS and hepatic encephalopathy.
For inpatients a platelet count between >20,000/µL and 50,000/µL was the most common pre-transfusion count (28% of all episodes) with similar results for general ward (29%) and ICU patients (35%). In the ED and OR a platelet count >100,000/µL was most common - found in 38% and 37% of all episodes. For outpatient transfusions a count of >10,000/µL to 20,000/µL was most common (25%). For inpatients post-platelet count increment ranged from a median of 12,000/µL to 23,000/µL with progressively larger increments seen with progressively higher starting counts (Table 1). For outpatients post-platelet count increments ranged from 21,000/µL to 27,000/µL (Table 1).
Conclusion: The REDS-III data base provides a wealth of information to assess platelet transfusion therapy in the U.S. Transfusion of more than 1 dose of platelets per episode is uncommon. Transfusion of ABO mismatched platelets is a common practice. Cardiovascular and Hematology -Oncology patients are prominent users of platelet products. General Ward and ICU dominate the location for platelet transfusion therapy and have similar transfusion practice patterns. The common pre-transfusion platelet count of 20,000-50,000/µL is surprising (as this exceeds evidence based recommendations for prophylactic transfusions in hematology-oncology patients) with reasons unclear. Platelet count increments were also surprisingly low. These findings, particularly the high pre-transfusion platelet count, the poor platelet increments and the high number ABO mis-matched transfusions, highlight differences in real world versus controlled studies and provide epidemiologic and laboratory data to develop future research to improve platelet transfusion practice.
Ness: Terumo BCT: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal